Splenic Trauma with Contrast Extravasation
- Sriya Kosaraju and Kevin Rice
- Apr 16, 2025
- 6 min read
A 61-year-old female presented with left upper quadrant abdominal pain and hypotension following a motor vehicle collision. How would you grade this injury? • Xray of the Week
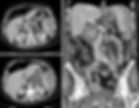
Figure 1. Contrast enhanced CT of abdomen and pelvis. How would you grade this injury? What action should be taken for this patient who is hemodynamically unstable?

Figure 2. Contrast enhanced CT of abdomen and pelvis demonstrating IV contrast extravasation from the spleen (red arrows). Note also the hematomas adjacent to the spleen and liver.

Figure 3. Initial selective splenic artery angiogram and subsequent coil embolization.
Discussion:
Splenic trauma occurs frequently in patients who sustain blunt abdominal injury, especially following high-energy mechanisms such as motor vehicle collisions. The injury can range from capsular tears to complete devascularization of the spleen. The American Association for the Surgery of Trauma (AAST) Splenic Injury Scale is a standardized grading system ranging from Grade I to Grade V used to classify the severity of splenic injuries based on imaging and surgical findings [1].
Imaging criteria for a Grade I injury includes subcapsular hematomas involving less than 10% of the surface area, parenchymal lacerations <1cm in depth, and capsular tear. Grade II injuries include subcapsular hematomas covering 10% to 50% of the surface area, intraparenchymal hematomas under 5 cm, or 1-3 cm lacerations (do not involve the trabecular vessels). Grade III injuries are characterized by subcapsular hematomas greater than 50% of the surface area or ruptured subcapsular or intraparenchymal hematomas larger than 5 cm, or lacerations deeper than 3 cm (involve the trabecular vessels) [1].
Grade IV injuries include lacerations that extend into segmental or hilar vessels and result in major devascularization of more than 25% of the spleen and any injuries with the presence of a splenic vascular injury or active bleeding within the splenic capsule. Since there is contrast extravasation, this is case is considered a Grade IV injury (Figs. 1-2). Grade V injuries are the most severe form, involving a shattered spleen or hilar vascular injury leading to devascularization of the organ and active bleeding extending beyond the spleen into the peritoneum [1]. Prompt identification of the injury grade is essential for guiding treatment decisions.
Higher-grade injuries (Grades IV and V), especially when accompanied by active contrast extravasation as in this case, typically indicate ongoing hemorrhage and necessitate urgent intervention, often through angioembolization or surgery. Lower-grade injuries (Grades I–III) can be managed non-operatively in hemodynamically stable patients [2].
Imaging:
Computed tomography (CT) is the imaging modality of choice for evaluating blunt abdominal trauma and identifying splenic injury. Contrast-enhanced CT, particularly with arterial and portal venous phases, allows for accurate detection and grading of splenic lacerations, hematomas, and vascular injuries. Key findings on CT include subcapsular and intraparenchymal hematomas, depth and extent of lacerations, active contrast extravasation, pseudoaneurysms, and areas of devascularization. Multiphase imaging increases sensitivity for detecting active bleeding, which appears as hyperdense contrast pooling in the arterial phase and persistent enhancement in delayed images. The sensitivity and specificity of contrast-enhanced CT in identifying clinically significant splenic injuries are both high, with CT also serving as the basis for injury grading using the AAST Splenic Injury Scale. Prompt and accurate identification of injury grade and vascular involvement is essential in guiding appropriate management, ranging from non-operative observation to embolization or surgery [3].
Treatment:
In this case, the patient presented with significant splenic trauma and active extravasation on imaging, which required urgent intervention. Given the hemodynamic instability and the severity of the injury, the patient underwent splenic embolization. Transcatheter arterial embolization (TAE) is considered the treatment of choice for high-grade splenic injuries and avoids the need for splenectomy in many cases. During embolization, selective catheterization of the splenic artery allows for precise delivery of embolic agents to the bleeding vessels, controlling the hemorrhage. It can successfully treat most splenic injuries with a low risk of complications. As an alternative to splenectomy, it is minimally invasive and effective in achieving hemostasis while preserving splenic function. However, patients with more severe injuries, such as complete splenic rupture or failure of embolization, may require splenectomy [4].
Prognosis:
Prognosis after splenic injury is dependent on degree of injury and time until treatment. Low grade injuries often have a very favorable prognosis, though delayed splenic rupture may occur up to 10 days post injury. The prognosis for patients undergoing TAE is generally favorable, especially in cases of successful embolization. When embolization effectively controls the bleeding, the patient can recover without the need for splenectomy and typically experience a full recovery. In up to 20% of patients, splenic infarction may occur after embolization (defined as more than 25% devascularization of the spleen). The risk of other complications such as recurrence of bleeding or abscess formation is low. However, patients who undergo splenectomy due to failed embolization or more severe injury are at higher risk for post-splenectomy infection, particularly with encapsulated organisms. This risk is highest in the first 2 years after splenectomy but can occur at any time. Vaccinations and long-term follow-up are essential in these patients. Early diagnosis, timely embolization, and careful post-procedural monitoring contribute to favorable long-term outcomes for most patients with splenic injuries [5].
References:
Injury scoring scale. The American Association for the Surgery of Trauma. (2025, Jan. 16). https://www.aast.org/resources-detail/injury-scoring-scale#spleen
Coccolini F, Montori G, Catena F, et al. Splenic trauma: WSES classification and guidelines for adult and pediatric patients. World J Emerg Surg. 2017;12:40. Published 2017 Aug 18. DOI: 10.1186/s13017-017-0151-4
Steven R Klepac, M. (2023, September 14). Splenic trauma imaging. Practice Essentials, Radiography, Computed Tomography. https://emedicine.medscape.com/article/373694-overview
Quencer KB, Smith TA. Review of proximal splenic artery embolization in blunt abdominal trauma. CVIR Endovasc. 2019;2(1):11. Published 2019 Mar 18. PMCID: PMC7224246 DOI: 10.1186/s42155-019-0055-3
Oelhaf RC, Sugumar K, King KC. Splenic Trauma. [Updated 2023 Jun 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430920/

Sriya Kosaraju is a medical student at University of Missouri-Kansas City (UKMC) School of Medicine and is pursuing radiology. Her interest is in the field radiology from its central role in patient care and the dynamic intersection of technology, innovation, and impactful clinical decision-making.
At UMKC, she currently serves as the Director of Research Initiatives for UMKC’s Vascular and Interventional Radiology Interest Group, where she helps organize journal clubs, connects students with mentors, and supports research opportunities in interventional radiology. She also serves as a Student Ambassador, guiding and mentoring prospective students through tours, panels, and other recruitment efforts.
On a national level, she currently serves on the Society of Interventional Radiology's membership committee and volunteers with both the Society of Interventional Radiology (SIR) and the American College of Radiology (ACR) Rad Reserves, contributing to projects to enhance radiology resources and outreach.
Sriya is passionate about preventative health care and the role of radiology in improving clinical outcomes. She is the founder and president of Mam4Mom, a nonprofit dedicated to increasing access to women’s health services. Through Mam4Mom, she has led initiatives including free mammogram and Pap smear days, community awareness campaigns, and care baskets for hospitalized cancer patients. She hopes to continue to explore ways to bridge medicine, service, education, and advocacy in her future career.
Follow Sriya Kosaraju on X (formerly Twitter) @sriyakosaraju

Kevin M. Rice, MD is the president of Global Radiology CME and is a radiologist with Cape Radiology Group. He has held several leadership positions including Board Member and Chief of Staff at Valley Presbyterian Hospital in Los Angeles, California. Dr. Rice has made several media appearances as part of his ongoing commitment to public education. Dr. Rice's passion for state of the art radiology and teaching includes acting as a guest lecturer at UCLA. In 2015, Dr. Rice and Natalie Rice founded Global Radiology CME to provide innovative radiology education at exciting international destinations, with the world's foremost authorities in their field. In 2016, Dr. Rice was nominated and became a semifinalist for a "Minnie" Award for the Most Effective Radiology Educator. He was once again a semifinalist for a "Minnie" for 2021's Most Effective Radiology Educator by AuntMinnie.com. He has continued to teach by mentoring medical students interested in radiology. Everyone who he has mentored has been accepted into top programs across the country including Harvard, UC San Diego, Northwestern, Vanderbilt, and Thomas Jefferson.
Follow Dr. Rice on X (formerly Twitter) @KevinRiceMD




















