Aortic Intramural Hematoma
- Han Ngo and Kevin M. Rice, MD
- Jul 6, 2020
- 4 min read
Updated: Feb 26, 2024
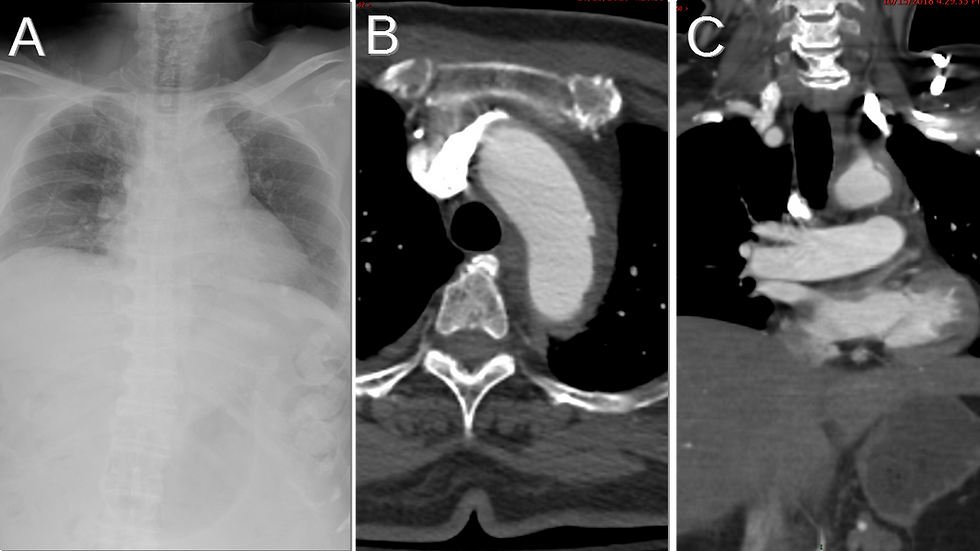
51M with hypertension and chest pain • Xray of the Week

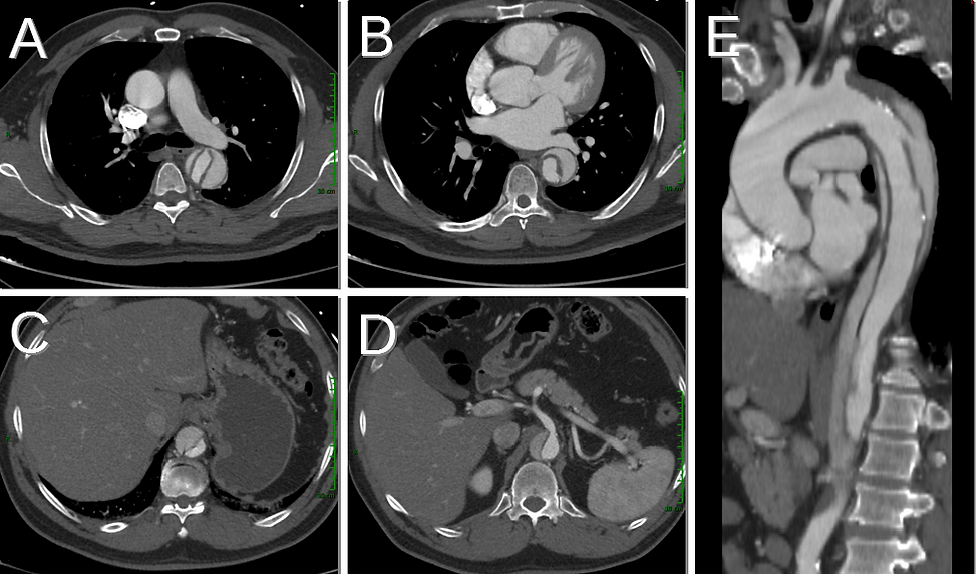
Figure 1. Name the important findings on this CT Scan.

Figure 2. CT of Stanford Type B aortic intramural hematoma.
A. Normal ascending aorta (green arrow). Note the crescent-shaped, hyperdense region along the wall of the descending aorta (yellow arrow) indicating intramural hematoma.
B. Normal ascending aorta (green arrow). The intramural hematoma is seen more inferiorly with an intramural blood pool demonstrated by contrast within the intramural hematoma without visualized connection to the lumen (blue arrow).
C. The intramural hematoma extends into the abdominal aorta on sagittal oblique MPR image (red arrow).

Figure 3. Diagram of Stanford classification for aortic intramural hematoma. Stanford A affects the ascending aorta, with or without descending aortic involvement and Stanford B affects the descending aorta, distal to the origin of the left subclavian artery. Diagram by Han Ngo.
Discussion:
Aortic dissection occurs when blood enters the aortic media due to an intimal tear. Aortic intramural hematoma (IMH), a variant form of the classic aortic dissection, originally was thought to occur due to hemorrhage within the aortic media from rupture of the vasa vasorum in the absence of an intimal tear (1,2). However, with the advent of high resolution imaging, intimal tears may be identified in patients with IMH. For this reason, it is postulated that aortic dissection has both an entry tear and an exit tear whereas IMH has only an entry tear (3) in the intima.
Older patients with history of hypertension are at highest risk for aortic dissection and IMH (4). Aortic dissection and IMH usually present with hypertension and chest pain that radiates to the back (3-6). IMH may progress to dissection, rupture, or acute cardiac tamponade occurred in up to 32% of cases (7). Acute aortic regurgitation may occur in up to 35% of patients with IMH (4,6,8). The Stanford classification system is used to categorize both aortic dissection and IMH (Fig. 3). Stanford Type A affects the ascending aorta, with or without descending aortic involvement and Stanford Type B affects the descending aorta, distal to the origin of the left subclavian artery (4,5). Usually Stanford Type A is treated surgically or with stent-graft placement while Stanford Type B is managed medically- primarily with blood pressure control (5-9).
On chest CT and MRI, aortic dissection is diagnosed by the presence of an intimal flap (1,2). With IMH, CT demonstrates a crescent-shaped hyperdense region along the aortic wall with no intimal flap (Fig. 2). This crescent sign represents the hematoma confined to the aortic media without visualized communication with the aortic lumen. As in this case, an intramural blood pool may be seen as enhancing blood in the aortic wall without visualized connection to the lumen, most often seen in the in the descending aorta (8, 10).
Followup imaging in patients with IMH is similar to that in patients with aortic dissection: CT or MR imaging done while in hospital and at 1, 3, 6, and 12 months after the initial presentation and then annually to evaluate for the emergence of complications (9).
References:
1. Song J-K. Diagnosis of aortic intramural haematoma. Heart. 2004;90:368-371. doi: 10.1136/hrt.2003.027607
2. Macura KJ, Corl FM, Fishman EK, et al. Pathogenesis in acute aortic syndromes: aortic dissection, intramural hematoma, and penetrating atherosclerotic aortic ulcer. AJR Am J Roentgenol. 2003;181 (2): 309-16. doi:10.2214/ajr.181.2.1810309
3. Gutschow SE, Walker CM, Martínez-Jiménez S, et al. Emerging Concepts in Intramural Hematoma Imaging. (2016) Radiographics : a review publication of the Radiological Society of North America, Inc. 36 (3): 660-74. doi:10.1148/rg.2016150094
4. Alomari IB, Hamirani YS, Madera G, et al. Aortic intramural hematoma and its complications. Circulation. 2014;129(6):711-716. doi:10.1161/CIRCULATIONAHA.113.001809
4. Herrán FL, Bang TJ, Thomas NR, et al. CT imaging of complications of aortic intramural hematoma: a pictorial essay. 2018. Diagn Interv Radiol. 2018 Nov; 24(6): 342–347. doi:10.5152/dir.2018.17261
5. Weis-Müller BT, Sandmann W. Aortic dissection. In: Vascular Surgery: Cases, Questions and Commentaries. Springer International Publishing; 2018:83-92.
6. Chao CP, Walker TG, Kalva SP. Natural history and CT appearances of aortic intramural hematoma. Radiographics. 2009;29 (3): 791-804. doi:10.1148/rg.293085122
7. Nienaber CA, von Kodolitsch Y, Petersen B, et al. Intramural Hemorrhage of the Thoracic Aorta Diagnostic and Therapeutic Implications. Circulation. 1995;92:1465–1472 doi:10.1161/01.CIR.92.6.1465
8. Gutschow SE, Walker CM, Martínez-Jiménez S, et al. Emerging Concepts in Intramural Hematoma Imaging. (2016) Radiographics : a review publication of the Radiological Society of North America, Inc. 36 (3): 660-74. doi:10.1148/rg.2016150094
9. Hiratzka LF, Bakris GL, Beckman JA et al. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with thoracic aortic disease: executive summary. J Am Coll Cardiol 2010;55(14):1509–1544. doi:10.1016/j.jacc.2010.02.010
10. Wu MT, Wang YC, Huang YL et al. Intramural blood pools accompanying aortic intramural hematoma: CT appearance and natural course. Radiology 2011;258(3):705–713. doi:10.1148/radiol.10101270

Han Ngo is a medical student at Oakland University William Beaumont School of Medicine (OUWB) in Rochester, Michigan. She graduated from UCLA, receiving her B.S. degree in Biochemistry. Prior to starting medical school, Han spent 4+ years (including her undergraduate years) working as a medical scribe for a psychiatrist at Ronald Reagan UCLA Medical Center. Interested in radiology, Han is now serving as the President of both diagnostic radiology and interventional radiology interest groups at OUWB. She is also a committee member on the Medical Student Council of the Society of Interventional Radiology (SIR). After deciding on her specialty, Han plans to continue learning and striving to make a difference in patients’ lives.
Follow Han Ngo on Twitter @Han_Ngoo

Kevin M. Rice, MD is the president of Global Radiology CME and is a radiologist with Cape Radiology Group. He has held several leadership positions including Board Member and Chief of Staff at Valley Presbyterian Hospital in Los Angeles, California. Dr. Rice has made several media appearances as part of his ongoing commitment to public education. Dr. Rice's passion for state of the art radiology and teaching includes acting as a guest lecturer at UCLA. In 2015, Dr. Rice and Natalie Rice founded Global Radiology CME to provide innovative radiology education at exciting international destinations, with the world's foremost authorities in their field. In 2016, Dr. Rice was nominated and became a semifinalist for a "Minnie" Award for the Most Effective Radiology Educator. He was once again a semifinalist for a "Minnie" for 2021's Most Effective Radiology Educator by AuntMinnie.com. He has continued to teach by mentoring medical students interested in radiology. Everyone who he has mentored has been accepted into top programs across the country including Harvard, UC San Diego, Northwestern, Vanderbilt, and Thomas Jefferson.
Follow Dr. Rice on Twitter @KevinRiceMD

















Comments